Although
these terms refer to several different diseases and causes, these have
clearly similar mechanisms and face the same therapeutical challenges
most of the time. Particularly Meibomian Dysfunctions, sometimes called
lid margin diseases, have many aspects in commun. For the most serious
cases, phlyctenular ulcerations may appear and lead to visual
impairment. As with most dysfunctional tear syndromes, the range in
severity and consequences may be very large. Corneal damage is clearly
one objective sign of severity in these diseases. These are usually the
consequence of a meibomian dysfunction affecting the lipid layer of
tears. In some situations, the deficient lipid layer may lead to
lipases, greasy agglomerates which block the glands and may become acid
and induce toxicity through the presence of bacteria. All types of lid
abnormalities may cause a dysfunctional tear film.
These are frequently encountered and
chronic pathologies but often orphan of proper care and drug. This will
hopefully change soon. Currently the only treatments are long-term doxycycline
per
os and sometimes topical antibiotherapy for severe episodes.
Meibomitis:
The term means inflammation of the Meibomius glands that is present in
several lid and ocular diseases. Most frequently the glands are clogged
due to an hypersecretion and pressing the glands may result in
extracting a thick liquid but even sometimes tooth-paste like substance
(when normally it would be a clear lipid liquid substance). When these
clogged glands are formed, bacterial lipases may in turn produce acid
grease that affects the physical and chemical properties of the tear
film. The tear film may then become irregularly greasy, foamy and will
tend to break very easily thus creating a dryness syndrome. As for
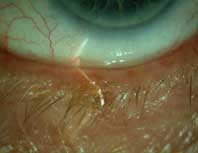
blepharitis, a more of less diffused lid margin inflammation with
telangiectases (dilated small
blood vessels) is seen around the Meibomian glands.
Anterior and
Posterior Blepharitis: Blepharitis
means inflammation of the lids. Blepharitis is one of most frequent
ocular annex disorders. Belpharitis
affects the lid margin, the eyelashes and the meibomian glands. There
are two types of blepharitis depending on its location: anterior
(eyelashes and external surface of the lids) and posterior (meibomian
glands and lid margin) and several types depending on etiology (allergic, fyngal, herpetic, seborrheic,
staphylococcic, viral, parasitay,
due to demodex, due to ocular
rosacea, etc). Blepharitis is characterised by swollen and red lids (telangiectases);
crusts and squamae (scale-like apparent bits of skin).
Anterior Blepharitis may not have an impact on the ocular surface.
Posterior Blepharitis has ocular surface incidences, and may notably
cause a meibomian dysfunction. Upon waking, the lids may become
sticky and are sometimes covered with crusts caused by the lipid
malfunction. The patient may suffer from irritation and foreign body
sensation. There is no cure for chronic blepharitis. There are many
possible consequences of blepharitis, including: chalazia, styes,
meibomitis, dry eyes, marginal ulcerations, trichiasis, etc.
Sebhorreic
Dermatitis: is a skin disease manifesting itself through
redness and squamae on the face (particularly near
the
hair limits, the brows and the eyelashes), which may affect the eye
notably through a meibomian dysfunction. This disesase is characterised
by redness or the eruption of red spots, yellowish greasy squamae, more
or less pruriginous, predominant in sebaceous glands-rich areas.
At the hair level dandruff is frequently seen.
Rosacea
& Ocular Rosacea:
Rosacea itself, is a skin vascular disease, also known as couperosis or
acnea rosacea, which may affect the eye. Rosacea is charactherised
by erubescent (sudden redness) paroxystic episodes and a erythemato-telangiectasic
state (couperosic state) of the face.
Inflammatory lesions may appear, mainy around the nose, the cheeks, the
front and the chin. Only the ocular aspects enter in the scope of
Keratos' actions. Ocular rosacea is usually noticeable through
blepharitis and conjonctivitis, but it may also lead to visual damage
due to ulcerations (usually marginal). In the latter situation a
phlyctenular keratoconjonctivitis causes a peripherical keratitis, and
possibly ulcerations and sometimes cicatricial astigmatism. This most
renown consequence, is fortunately not the most commun aspect of
rosacea. The most common symptoms are chronic conjonctivitis and
blepharitis. There is no cure for both rosacea and ocular rosacea.
Lib
abnormalities and "mechanical disorders".
Other lid conditions may lead to
ocular dryness and favour erosions, either through direct expose to the
air (in the absence of an adequate tearfilm) or due to mechanical
friction such as lagophtalmos (incomplete
closure of the lid leaving the eye partially exposed), or abnormal lids
as in ectropion and
entropion, stye and chalazion.
Identically, an eye that suffered a trauma may change its shape. Eyelids
suffering from these anatomical changes may irritate or harm the cornea
through constant blinking and friction with cornea.
Trichiasis, is another of such conditions
where, misplaced eyelashes may groz torward the eye or the cornea and
harm its tissues.



From left to right, pictures of eyelids
presenting chalazion, entropion with trichiasis, and ectropion
respectively by
Dr Edouard Benois.
▲

copyright ©
Keratos 2005-2007